Ovulation: A Comprehensive Guide
It’s no secret that women are incredible. Creating and caring for a child inside their body for 9 months – I’m continually in awe of the female body. And this fascination led me to ask the question, “What exactly happens during ovulation?” Ovulation, a fascinating and intricate process within the female body, plays a pivotal role in human reproduction. Understanding the nuances of ovulation is crucial for women who are trying to conceive or simply want to comprehend the complexities of their own bodies! You. are. simply. amazing.

In this article, we will delve into the intricacies of ovulation, exploring what it is, how it occurs, and the various physiological changes that take place within the female body during this crucial phase.
Explaining Ovulation
Ovulation, the cornerstone of female fertility, refers to the release of a mature egg from the ovary into the fallopian tube, where it awaits fertilization by sperm. This pivotal event occurs approximately once every menstrual cycle, usually around the middle of the cycle, although slight variations can occur. The process is meticulously regulated by a complex interplay of hormones and physiological changes.
The process starts in the ovaries where a dominant follicle emerges. The dominant follicle is a fluid-filled sac that develops within the ovary. Each menstrual cycle, multiple follicles begin to develop in the ovary under the influence of follicle-stimulating hormone (FSH) released by the pituitary gland.
Out of these developing follicles, one follicle becomes the dominant follicle, meaning it grows and matures more rapidly than the others. The selection of the dominant follicle is a result of complex hormonal interactions and genetic factors.
The dominant follicle contains an immature egg, also known as an oocyte, surrounded by a cluster of specialized cells called granulosa cells. These cells provide nourishment and support to the developing egg. As the dominant follicle continues to grow, it increases in size and reaches its maximum diameter, typically around 20-25 millimeters.
Growth Phase Explanation
During this growth phase, the dominant follicle produces increasing amounts of estrogen, a hormone that plays a key role in preparing the uterus for potential pregnancy. The rising estrogen levels signal the hypothalamus and pituitary gland to reduce the secretion of FSH, preventing the development of other follicles. This ensures that all the available resources and hormonal support are directed towards the maturation of the dominant follicle.
Once the dominant follicle reaches its mature stage, it undergoes the process we know as ovulation. This occurs due to a surge in luteinizing hormone (LH) released by the pituitary gland, which triggers the final stages of follicle development. The LH surge causes the follicle to rupture, releasing the mature egg into the pelvic cavity. The fimbriae, finger-like projections at the end of the fallopian tubes, then sweep over the ovary to capture the released egg and guide it into the fallopian tube for potential fertilization.
If the egg is fertilized by sperm during its journey through the fallopian tube, it implants into the uterine lining, leading to pregnancy. However, if fertilization does not occur, the corpus luteum, a structure that forms from the remnants of the ruptured follicle, begins to produce progesterone. Progesterone prepares the uterine lining for implantation but gradually decreases if pregnancy does not occur, initiating menstruation and the start of a new menstrual cycle.
The Female Reproductive System During Ovulation
The female reproductive system undergoes several remarkable changes during ovulation. These changes work in harmony to facilitate the release, transportation, and potential fertilization of the egg.
- The Ovaries: Within the ovary, a fluid-filled sac called the dominant follicle gradually develops and matures. This follicle houses the egg, which is surrounded by a cluster of cells. As ovulation approaches, the dominant follicle ruptures, releasing the egg into the pelvic cavity.
- The Fallopian Tubes: Upon ovulation, the fimbriae, finger-like projections at the end of the fallopian tubes, sweep over the ovary to capture the released egg. These delicate structures create a gentle current that helps guide the egg towards the fallopian tube, where it awaits fertilization by sperm.
- The Cervix: The cervix, a most under-appreciated female organ, is the lower part of the uterus and undergoes changes during ovulation. It produces a thin, slippery mucus that facilitates the passage of sperm through the cervix and into the uterus. This fertile cervical mucus provides a friendly environment for sperm survival and motility.
- The Uterus: In preparation for a potential pregnancy, the lining of the uterus, known as the endometrium, thickens during the menstrual cycle. If fertilization occurs, the fertilized egg implants itself into this nourishing lining. During ovulation, the uterus also experiences mild contractions that help propel sperm towards the awaiting egg.
Symptoms During Ovulation
Many women experience specific symptoms during ovulation, providing clues to the occurrence of this crucial phase. While not all women may notice these symptoms, common signs include:
1. Changes in Cervical Mucus
The consistency and appearance of cervical mucus change during ovulation. It becomes clear, stretchy, and more slippery, resembling the consistency of egg whites. This change is conducive to sperm survival and facilitates their journey through the reproductive tract. During ovulation, the cervix undergoes specific changes that result in alterations in cervical mucus. Cervical mucus is a fluid secreted by the cervix, the lower part of the uterus that connects to the vagina. It serves several important functions in the female reproductive system, including facilitating the transport of sperm through the cervix and into the uterus.
As a woman approaches ovulation, the composition and consistency of cervical mucus undergo significant changes under the influence of hormonal fluctuations, particularly rising estrogen levels. These changes are collectively referred to as the “fertile cervical mucus.”
At the beginning of the menstrual cycle, after menstruation, cervical mucus is typically minimal and thicker. This creates a barrier to sperm penetration. However, as ovulation approaches, estrogen levels increase, causing the cervical glands to produce more mucus and altering its quality.
Fertile cervical mucus is characterized by several distinct qualities:
- Increased Amount: The volume of cervical mucus significantly increases during ovulation. It becomes more abundant and noticeable compared to other phases of the menstrual cycle.
- Clear and Watery: Fertile cervical mucus becomes clearer, more transparent, and watery in consistency. It often resembles raw egg whites, having a slippery and stretchy texture.
- Stretchiness: One of the key characteristics of fertile cervical mucus is its stretchiness or spinnbarkeit. When a woman observes this type of mucus, she can stretch it between her fingers without it breaking easily.
- Lubrication: Fertile cervical mucus provides natural lubrication, making it easier for sperm to swim through the reproductive tract. This slippery texture helps sperm to survive and navigate towards the awaiting egg.
The changes in cervical mucus serve an essential purpose in promoting fertility. The watery and stretchy nature of fertile cervical mucus aids sperm in their journey through the cervix and into the uterus, increasing their chances of reaching the fallopian tubes where fertilization occurs. Tracking cervical mucus can even be an effective form of natural birth control.
2. Increased Libido
During ovulation, many women experience a noticeable increase in libido or sexual desire. This heightened sexual interest can be attributed to various physiological and hormonal factors. These factors occur during this phase of the menstrual cycle.
One key hormone involved in the regulation of ovulation and libido is estrogen. As the dominant follicle develops and matures, it produces increasing amounts of estrogen. Estrogen levels peak just before ovulation, triggering the release of luteinizing hormone (LH) and the subsequent release of the egg. This surge in estrogen not only stimulates the process of ovulation but also has a direct impact on sexual desire.
Estrogen has several effects on the body that can contribute to an increased libido. Firstly, it enhances blood flow to the pelvic area, including the genital region, leading to heightened sensitivity and arousal. Increased blood flow can result in engorgement of the clitoris and vaginal tissues, making sexual stimulation more pleasurable.
Secondly, estrogen influences the production of neurotransmitters such as serotonin and dopamine, which play key roles in mood regulation and sexual arousal. Elevated estrogen levels can enhance the release and uptake of these neurotransmitters, leading to improved mood and an overall heightened sense of well-being, which can positively impact sexual desire.
Additionally, hormonal changes during ovulation can affect the sense of attractiveness and desirability. Research suggests that women may experience increased self-confidence and attractiveness during this phase of their cycle, potentially influencing their sexual interest and behavior.
3. Ovulation Pain or Mittelschmerz
Ovulation pain, also known as Mittelschmerz (a German term meaning “middle pain”), refers to a mild twinge or cramp-like discomfort that some women experience during ovulation. It typically occurs on one side of the lower abdomen and may last for a few minutes to a few hours. While not all women experience Mittelschmerz, it is estimated that around 20% of women may notice this ovulation-related pain.
The exact cause of Mittelschmerz is not fully understood, but several theories have been proposed. One explanation is that the pain results from the stretching or rupture of the ovarian wall as the dominant follicle releases the mature egg during ovulation. The release of the egg, along with the release of fluid and blood into the pelvic cavity, may irritate the surrounding tissues, leading to discomfort.
Another theory suggests that the pain may be due to the contraction of the fallopian tubes or the release of prostaglandins, hormone-like substances that play a role in various physiological processes, including pain perception. These contractions and the release of prostaglandins could cause mild inflammation or irritation in the pelvic area, resulting in the sensation of pain.
Intensity and Duration of Mittelschmerz
The intensity and duration of Mittelschmerz can vary from woman to woman. Some may experience only mild discomfort, while others may have more pronounced pain. The pain is usually localized to one side of the lower abdomen, corresponding to the ovary that released the egg. In some cases, the pain may alternate sides from cycle to cycle.
It is important to note that Mittelschmerz is typically considered a normal and benign occurrence. However, if the pain is severe, prolonged, or accompanied by other concerning symptoms, it is advisable to consult a healthcare provider. This is to rule out any underlying conditions or complications.
Monitoring and tracking ovulation-related pain can be helpful for women who are trying to conceive, as it may serve as an indicator of the timing of ovulation. Additionally, awareness of Mittelschmerz can provide reassurance to women who experience this discomfort, as it confirms the occurrence of ovulation and the healthy functioning of the reproductive system. As with menstrual cramps, the best pain relief technique is heat.
Shop Pixie Cup’s Eva Thermal. This cordless heating pad is portable and discreet, easily hidden under clothing. So whether you’re cramping or dealing with mittelschmerz, the Eva Thermal is the warm hug that you need to experience pain relief.

4. Breast Tenderness
Breast tenderness during ovulation is a common symptom experienced by some women. This discomfort, often described as breast soreness or sensitivity, can occur in one or both breasts. It is believed to be related to hormonal fluctuations that take place during the menstrual cycle.
The primary hormone involved in breast tenderness during ovulation is estrogen. The rise in estrogen levels during ovulation can cause breast tissue to retain fluid, leading to swelling and increased sensitivity.
In addition to estrogen, other hormones such as progesterone and prolactin may also contribute to breast tenderness. Progesterone levels increase in the second half of the menstrual cycle, after ovulation, and can further exacerbate breast discomfort. Prolactin, a hormone involved in milk production, may also rise during ovulation, potentially leading to breast changes and tenderness.
The exact mechanisms through which these hormones cause breast tenderness are not fully understood. However, they are believed to influence the sensitivity of breast tissue and the responsiveness of breast cells to hormonal signals. The increased fluid retention, hormonal fluctuations, and changes in breast tissue can collectively contribute to breast tenderness during ovulation.
In conclusion, the process of ovulation showcases the incredible capabilities of women’s bodies! The intricate hormonal orchestration, the precise development and release of the dominant follicle, the synchronized changes in the reproductive organs, and the accompanying symptoms all highlight the remarkable complexity and functionality of the female reproductive system. Ovulation is a powerful reminder of women’s unique ability to conceive and bring new life into the world and is a testament to the strength, resilience, and beauty of the female body. Embracing and understanding the intricacies of ovulation empowers women to appreciate their bodies, embrace their fertility, and embark on the remarkable journey of reproduction.
Our Top Picks For You
-
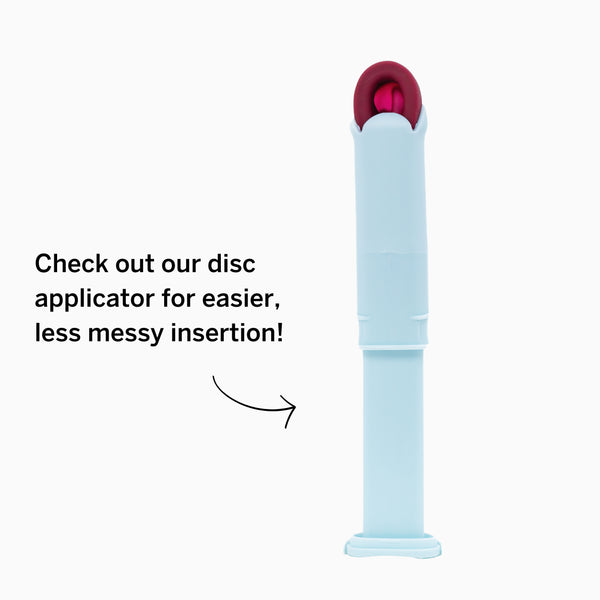
Period Disc & Applicator Kit
![]()
- Regular price
- $35
- Sale Price
- Regular price
-
$55 - $35
- Unit price
- per
Sold out -
Reusable Organic Cotton Pads
![]()
- Regular price
- $25
- Sale Price
- Regular price
-
$34 - $25
- Unit price
- per
Sold out -
Disposable Organic Cotton Pads
![]()
- Regular price
- $7
- Sale Price
- Regular price
-
$9 - $7
- Unit price
- per
Sold out -
Combo Disc + Applicator Bundle
![]()
- Regular price
- $39
- Sale Price
- Regular price
-
$49 - $39
- Unit price
- per
Sold out