PMS symptoms are common, but not normal
At the doctor’s office, they will take your temperature, pulse, blood pressure, and respiratory rate and they may even ask, “when was your last period?” For a long time, I would nonchalantly guess when my last menses was, and the doctor would say “great” and move on.
What if the doctor asked “how was your last period?” or “Any breast tenderness, mood swings, pain, or anxiety leading up to your period?” This would be a very different, and helpful conversation.

As a society, we have to understand that periods are a key indicator of women’s health. A recently reaffirmed committee opinion by ACOG and the American Academy of Pediatrics (AAP) advises health practitioners to consider periods the “fifth vital sign” — meaning healthy menstrual cycles without PMS/PMDD are as important a health indicator as changes in body temperature, pulse, breathing rate, and blood pressure (Varta, 2020).
Healthy menstrual cycles without PMS/PMDD are as important a health indicator as changes in body temperature, pulse, breathing rate, and blood pressure.
What does PMS stand for?
PMS has been the butt of many jokes, but PMS jokes are not funny, period (see what I did there). All jokes aside, PMS does not stand for “Please meet satan,” “Pardon My Sobbing,” or “Pass My Sweats.”
PMS, Premenstrual Syndrome, has been misunderstood for a very long time, and a lot of women have been or will be dismissed by physicians when they have legitimate PMS symptoms.
How common is PMS?
Over 85% of menstruating women in the United States experience PMS. (Romm, 72); PMS may be common, but it is not normal! To all the women who believe you have lost agency over your body or have a design flaw, please repeat after me… I AM DESIGNED TO DOMINATE. We do not have to be afraid of that time of the month. We can actually get to a place where we look forward to a time in our cycle where we can slow down and appreciate what our bodies can do.
How do I know if I have PMS?
PMS is a myriad of physical and emotional symptoms that will arise 2-10 days before the start of your menses (Day 1 of full flow). PMS symptoms can be a result of hormone imbalance or poor interaction between sex hormones, stress hormones, and neurotransmitters (chemicals controlling your mood) (Romm, 73).
The timing of the symptoms will typically be consistent to the individual woman. Charting your cycle may help you to proactively address your symptoms (Weschler 2015, 315). For example, after charting your cycle for a few months, you may notice that you always feel irritable three days before the start of your period. Being aware of this can help you be more mindful of your irritability so that you don’t take it out on those around you.
Questions answered on this page: How many days before your period do you get PMS?
What are the symptoms of PMS?
There are around 150 physical, behavioral, emotional, and cognitive symptoms that have been designated to PMS (see table below). The criteria to diagnose PMS is not a hard and fast science, but there is general agreement that if you have 5 or more of the symptoms mentioned below, in the “PMS Assessment,” 2-10 days before your period, and they resolve after your flow starts, then it is technically PMS.
Types of PMS symptoms
| Affective | Depression, irritability, anxiety, anger, weepiness, panicky feelings |
| Behavioral | Impulsive actions, compulsions, agitation, lethargy, decreased motivation |
| Autonomic | Palpitations, nausea, constipation, dizziness, sweating, tremors, blurred vision, hot flashes |
| Fluid/Electrolyte | Bloating, water-weight gain, breast fullness, hand and foot swelling |
| Dermatological | Acne, oily hair, hives, rashes, herpes, and allergy outbreaks |
| Cognitive (Brain) | Decreased concentration, memory changes, word-retrieval problems, fuzzy thinking, foggy-brain feelings |
| Pain | Migraines, tension headaches, back pain, muscle and joint aches, breast pain, and neck stiffness |
PMS Assessment
One or more of the following:
- Mood swings, weepiness, unexplained sadness
- Unexplained anger, irritability
- Depression, toxic self talk
- Tension, anxiety, wired+tired
Plus one or more of the following:
- Inability to focus
- Abnormal changes in appetite, food craving, binge eating
- Lack of interest in normal activities
- Unexplained fatigue, lack of energy
- Feeling overwhelmed
- Breast tenderness, bloating, weight gain, joint.muscle pain
- Sleep disturbances
Does PMS get worse with age?
PMS primarily affects women over the age of 25 and tends to get worse with age or after pregnancy and birth. This does not mean younger women cannot experience PMS symptoms. During the first few years of menstruation, hormonal “rivers” are being carved out, so it may take time to establish a “normal” for younger women.
Is PMS normal?
As I mentioned before, 85% of menstruating women in the US experience PMS symptoms, but PMS is not “normal” and should never be treated as such.
What is normal? It is normal to have subtle signs and symptoms that your period will begin soon, but if those subtleties turn into interferences in your life, then you are dealing with PMS.
Which is worse, PMS or PMDD?
PMS also has a bigger and badder sister called PMDD (Premenstrual dysphoric disorder). PMDD affects 3-8% of women worldwide and the symptoms are severe enough to cause debilitating physical, emotional, and psychological effects that affect relationships, careers, and mental well-being (Jardim, 48).
What is PMS/PMDD caused by?
PMS and PMDD signs and symptoms range in severity because they are highly influenced by our nutrition, stress management, gut health, and blood sugar balance, which can all lead to estrogen dominance if not kept in check.
What hormone is responsible for PMS/PMDD?
Estrogen is a queen sex hormone, but she can become a clingy friend that dominates the relationship. Estrogen dominance is when estrogen dominates over progesterone in the second half of your cycle, the luteal phase.
As Nicole Jardim, author of Fix Your Period, says, progesterone is our “Keep Calm and Carry On” hormone (2020, p.48). Both estrogen and progesterone influence the chemicals in our brain (neurotransmitters), such as serotonin, dopamine, and oxytocin. These neurotransmitters affect our mood, so it makes sense that if our imbalanced hormones are negatively affecting our neurotransmitters, that we would experience mood swings as a PMS/PMDD symptom.
Is PMDD considered a mental illness?
For PMDD, selective serotonin reuptake inhibitors (SSRIs) are typically prescribed because the DSM-5 has declared PMDD a psychiatric condition.
SSRIs are a widely used type of antidepressant. They are most commonly prescribed to treat depression, especially in severe cases like PMDD.
Now, I am not saying that this isn’t an appropriate medical approach, but I think it is missing the bigger picture. Conventional medicine and functional medicine would be the perfect combination to tackle PMS/PMDD, and to break the narrative that our symptoms are all in our head.
What can be done to address PMS/PMDD symptoms?
Addressing hormone imbalances is never a “peel-and-stick” situation, but there are basic functional approaches that every menstruating woman can take to live in hormonal bliss:
Jump off the blood sugar roller coaster
Insulin is a queen hormone and she deserves to be treated as royalty. Insulin is in charge of keeping blood sugar balanced, but when we are constantly stressed or eating poorly, then we continue to stay on the blood sugar roller coaster. High blood sugar and insulin levels are directly and indirectly linked to PMS, PCOS, endometriosis, fibroids, and heavy / painful periods. How do we get off of the blood sugar roller coaster?
Include these at every meal:
- 4-6 ounces of animal or plant-based protein
- 2 cups of colorful veggies. Eat the rainbow!
- 1 serving of slow carbs such as grains or an energy veggie like sweet potato
- Healthy fat (1 T olive oil, ½ avocado)
Love your liver
Our bodies are always seeking balance, and one way to achieve balance is through the liver. The liver plays a major role in detoxification and elimination pathways. The detoxification process starts in our liver, where used up or excess hormones are filtered and metabolized. How do we love our livers?
- Add cruciferous vegetables to your diet (broccoli, brussel sprouts, cabbage, kale, etc.)
- Supplement with DIM (diindolylmethane) in your luteal phase to help the liver with detoxification. The luteal phase is the phase of your cycle that begins after ovulation and lasts until menstruation begins.
- Drink dandelion root and ginger tea.
Eliminate endocrine disrupting chemicals
Endocrine disrupting chemicals (EDCs) are compounds that harm the natural rhythm of our endocrine system. They can mimic our natural hormones, and have been linked to health issues such as infertility, endometriosis, certain cancers, and — you guessed it — PMS symptoms. Estrogen-mimicking compounds, known as xenoestrogens, are present in BPA, parabens, phthalates, pesticides, and herbicides. How do we start to eliminate EDCs out of our lives?
- Buy clean cosmetic products that don’t contain parabens or phthalates
- Buy or make natural cleaning products
- Eat foods that are not processed with pesticides, hormones, or antibiotics
- Get rid of plastic food containers and water bottles
- Avoid fragrances and switch to essential oils
Get good with your gut
The gut-hormone connection is truly amazing and has been the focus of more and more scientific research. Because gut health has a direct effect on hormone health, it also has a direct effect on mental health. Our gut is responsible for eliminating excess hormones like estrogen out of our bodies. What can you do to address gut health?
- Possibly have a panel done to identify problematic foods so you can eliminate them from your diet
- Limit inflammatory foods such as sugar, caffeine, alcohol, and vegetable oils
- FIBER! Fiber feeds our guts and give our good bacteria what they need to flourish
- Manage stress levels
- Look into a good probiotic
Fill in the gaps in your diet
In today’s world, it is really hard to get all of our nutrients from the foods we eat, so it’s important to take a quality multi/prenatal vitamin to fill in our nutrient gaps. Along with a multi/prenatal vitamin, you may also need extra supplemental support due to your specific needs. Always talk to your doctor before starting new vitamins or herbal supplements.

Resources:
Jardim, N. (2020). Fix Your Period (1st ed.). HarperCollins.
Romm, A. (2021). Hormone Intelligence (1st ed.). HarperCollins.
Varta, S. J. (2020). Doctors Think Your Period Should Be a Fifth Vital Sign
Weschler, T. (2015). Taking Charge of Your Fertility (20th ed.). HarperCollins.
Our Top Picks For You
-
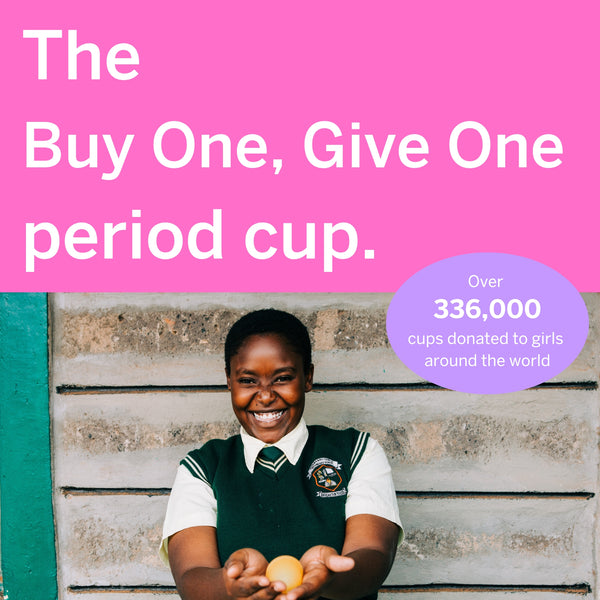
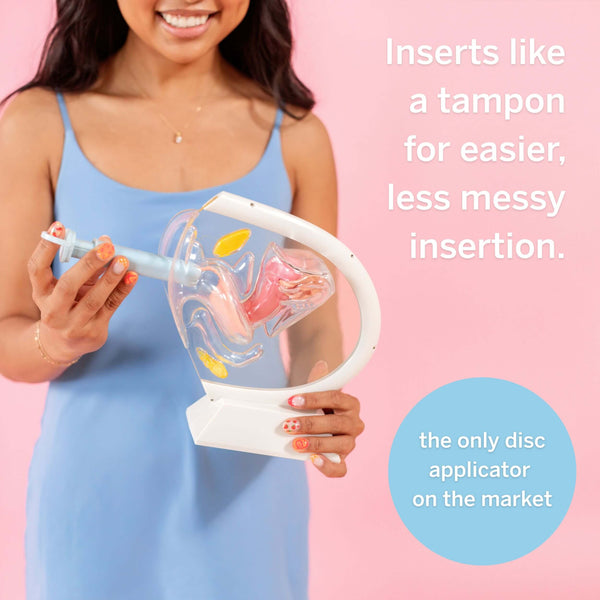
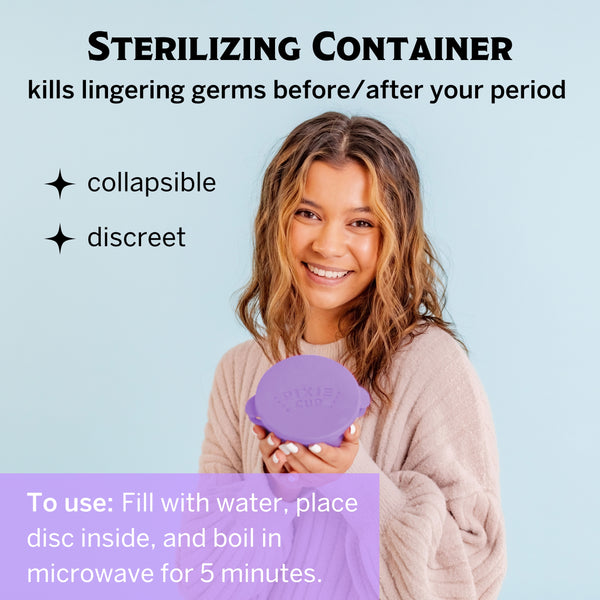
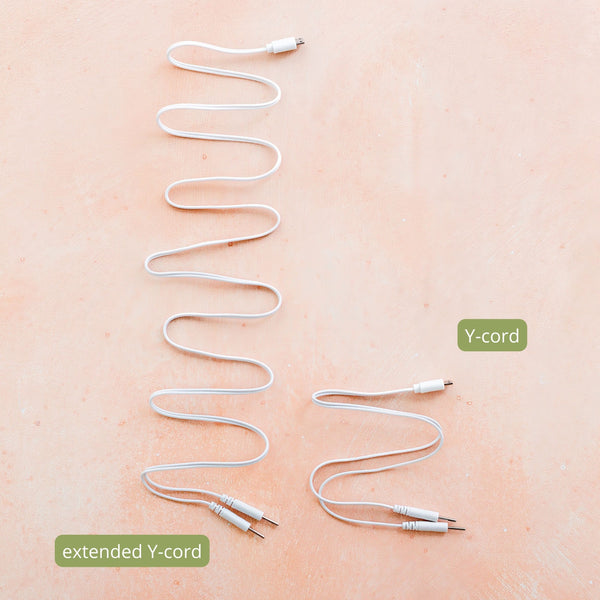
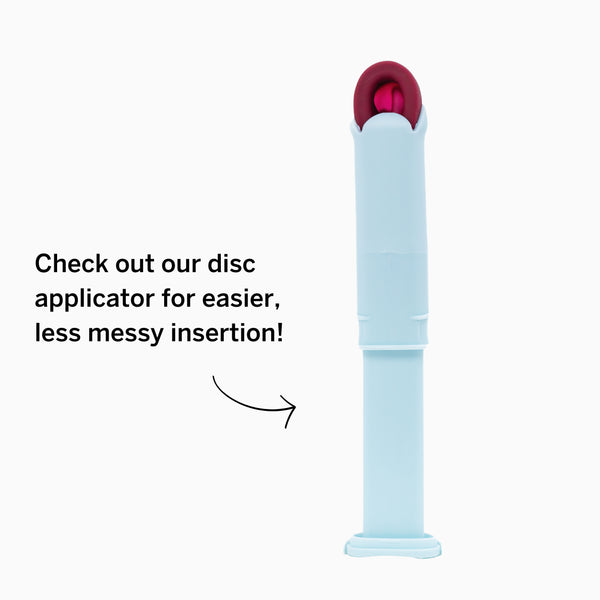
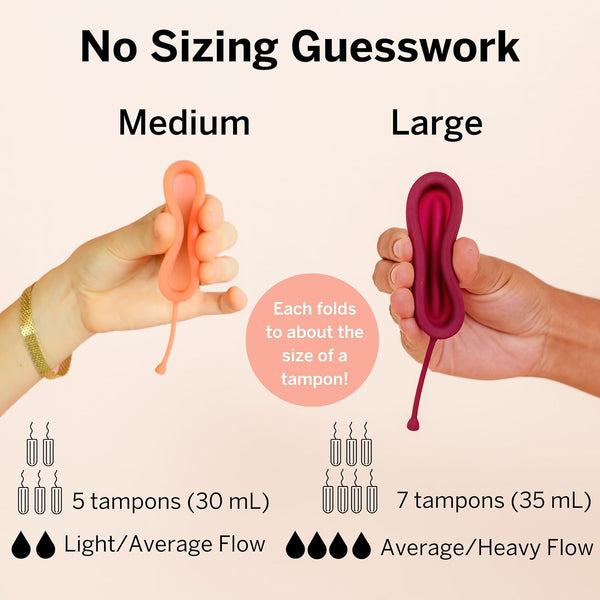
Period Disc & Applicator Kit
![]()
- Regular price
- $48
- Sale Price
- Regular price
-
$55 - $48
- Unit price
- per
Sold out -
Reusable Organic Cotton Pads
![]()
- Regular price
- $28
- Sale Price
- Regular price
-
$34 - $28
- Unit price
- per
Sold out -
Disposable Organic Cotton Pads
![]()
- Regular price
- $7
- Sale Price
- Regular price
-
$9 - $7
- Unit price
- per
Sold out -
Combo Disc + Applicator Bundle
![]()
- Regular price
- $42
- Sale Price
- Regular price
-
$49 - $42
- Unit price
- per
Sold out